Prepare yourself for a LONG read with pictures. 😉
It all began the day before we left for South Padre. You see, we have a cute waterfall pond that’s filled about 8 goldfish. On that day, the pond pump decided to quit working. So, off to Lowe’s K went. It was a good thing that the pump died because K decided to check out the Inverters that Lowe’s had available. When he found them, he FaceTimed me to check the voltage & amps/watts my Bipap runs on. He bought one so that I could use my bipap while in the van!
Our vacation was pretty adventurous from the very beginning. It first started with my oxygen reservoir we keep in our van for car rides. It decided to start leaking oxygen when we got there. We called Life Support-Dallas, who services my oxygen needs, and K and Eddie (Life Support) walked through through on FaceTime trying to fix it. Well, K did everything right but when he poured hot water on the chunk of ice that was around the leak, the hose snapped off. All the liquid oxygen bled out. See what happened! (Large video 30mb) https://livingono2forlife.files.wordpress.com/2022/10/img_2536.mp4
Naturally we scrambled to calculate how much oxygen I had left and how many refills my portables can use from one of my 2 100lb reservoirs in the condo before we had to go home. Yikes. That was interesting. One of my tall reservoirs can fill both portables 12 times. Then we worried about the hurricane and which direction it was going to go. We made the decision to leave early if it came our way. Plus, we decided, when both reservoirs got down to 1/4 full, we would start for home since we no longer had my van reservoir to drive home on.
The next day, I asked K if he wanted me to tie a string around his glasses with a little duct tape (I never leave home without duct tape!). He said no because he didn’t want to look like a hill billy. Lol! 30 minutes later, he came back all upset because he lost his glasses in the Gulf. Men and their stubbornness… Am I right ? Lol! Ok so we scrambled to find an optometrist in the area who would see him the next day (Sunday). The doctor turned out to be super nice. We got a prescription and emailed it to K’s eye doctor where we get our glasses made. His glasses are super complex. All the bells and whistles on it. *rolling my eyes* So, his glasses are in the works while we wereon vacation. YAY!
Next, K get stung by a Blue Button jelly fish. My Go-Bag to the rescue again with Medical supplies this time. He’s fine. No real damage to report on that other than slight swelling. Wheww! I was like, Dude… don’t even say… “What could happen next.” Seriously, with his vacation track record.. I was fearing the worst! Well, the drama calmed down and we had a good time. He went to the beach every day and walked the dogs a bunch. Willow became our beach dog who chased the little hermit crabs and seagulls. Neither dog wanted anything to do with the water which was ok with me.
The water heater in the condo was not functioning properly. We had lukewarm showers and I had to heat water to hand wash the dishes (no diswasher). The night K lost his glasses in the Gulf, he went down with a flashlight to look for them along the water and found a $500 boombox bluetooth speaker system floating in the water! Wow! He was all excited. I posted information on Facebook in the SouthPadre Concierge and no one claimed it. K brought it home with us.
We went to the Fire Station to check out the Mobi-chairs (wheelchair for the beach that has large fat tires!) that we could’ve checked out for free to help me get down to the beach. However, we tried my wheelchair down the boardwalk to the sand, parked it at the end, and I could walk the rest of the way slowly. So, we didn’t need the Mobi-chair. It’s nice to have one available for free if I needed one though. The fire fighters were super nice and said they had oxygen if I needed it. I don’t think they realize just how much oxygen I use even though we told them 8lpm 24/7. *shrug* =o)
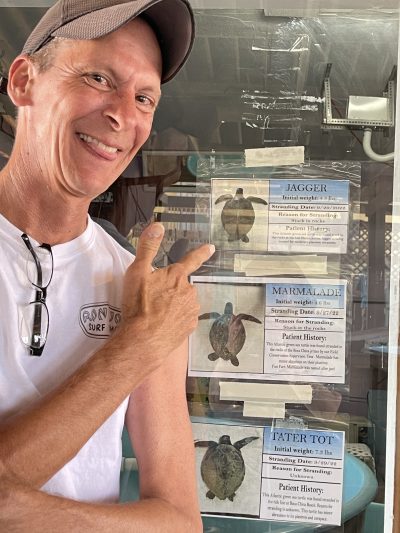
We went down to the Jetties where the shipping channel is. We watched the surfers catch a few of the higher waves that the hurricane had caused. We had a few red flag days there at the end for the water danger. That is where K went for a walk down the rocks of the jetty and found a turtle stuck head down between two massive rocks. Poor thing. We tried to let people know who where there but they all said not to touch it.. talk of big fines.. blah blah blah. So, he came and told me and we looked up the Sea Turtle Rescue place that we visited the day before and got them to come out to get the turtle out.
K got to name him Jagger (after Mick Jagger, of course!). They wouldn’t let him name him after Mike Modano (Dallas Stars!). We went back a few days later and checked on Jagger. He was doing well. Hope to watch his release on Facebook when the time comes. Every Friday and Saturday night we would go out on our patio when it got dark and a restaurant would set off fireworks that lasted about 5 mins. It was great!
We had a great time. I felt a little weird driving with my Bipap on. I’m just glad that K had to go to Lowe’s before we left for vacation because he found the inverter I could use to plug in my Bipap and use in the van. I don’t think I would have made it there and back without the use of my Bipap during the drive. My breathing has become very challenging now. I use a Bipap almost all day and night now.
[Health Update] I am going to contact my Sleep Lab doctor to get the ball rolling on getting me the more advanced machine called Trilogy. It can run on batteries or be plugged in and it’s mobile. I could use it anywhere in the house or in the car. It’s time to take that next step. K is slowly adjusting to my new health limitations. I’m proud of him because I know this isn’t easy for him at all. I just had my Telehealth visit with my Pulmonary Hypertension doctor. Everything we are doing is right. It’s just with age and progression of my limited ability to breathe, I’m happy that my heart is holding up as well as it has been. My lung volume has dropped. So, using the Bipap as much as I do now will keep the CO2 at a lower level. My next step will be getting an Echocardiogram (for internal blood pressures & chamber sizes) and a CT Scan on my ascending aorta aneurysm. I’m not a surgical candidate for fixing the aneurysm. There’s nothing they can do for it … just monitor it. It’s definitely past their criteria for surgical intervention. I am worried about it but I can’t spend my life worried about it. Just keep living life as much as possible and fill it with fun things to do.
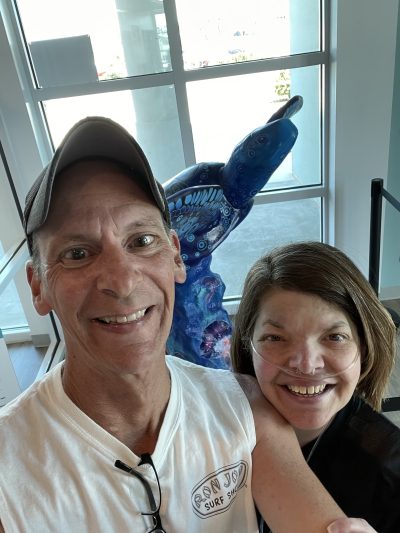
I hope you all are doing well. Here’s a few pictures we took. We went on a painted turtle scavenger hunt!